Authored by: Abt's National Health Workforce Collaborative Team
Rural healthcare in America depends on a workforce that is well-trained, supported, and integrated with the community. Yet 92% of rural counties are designated primary care shortage areas—many with five or fewer physicians, and some with none at all.i Additionally, two-thirds of mental health shortage areas are in rural regions.ii, iii
Workforce shortages lead to delayed care, higher rates of chronic disease, lack of adequate maternal care, and preventable deaths.iv For states, addressing workforce gaps is not optional; it’s foundational to improving health outcomes and sustaining rural economies.
States now have a historic opportunity: The federal Rural Health Transformation Program (RHTP) will invest $50 billion over five years to strengthen rural systems. The question is how to invest in strategies that recruit and retain workforce, redesign care, and rebuild trust.
Why Health Centers Are Crucial
Health centers are the backbone of community-based healthcare, serving over 32 million patients in the U.S. and providing a vital source of primary care in medically underserved areas.v In rural communities, health centers are often the only access point for care—not just for medical needs but for behavioral health, dental, and social services. Unfortunately, workforce shortages affect health centers more significantly than other types of healthcare organizations because they have limited resources to offer competitive salaries.vi Other barriers include:
- Lack of learning opportunities, infrastructure, trainers, and space for clinical rotation and placements
- Limited housing, childcare, and amenities
- Scarce spousal employment opportunities
- High provider burnout and behavioral health needs among staff
What We Heard from Rural Health Centers
Through the Health Resources and Services Administration (HRSA) National Health Workforce Collaborative, Abt engaged more than 900 stakeholders across all 10 HRSA regions—including 300+ health centers—to surface barriers and promising practices.
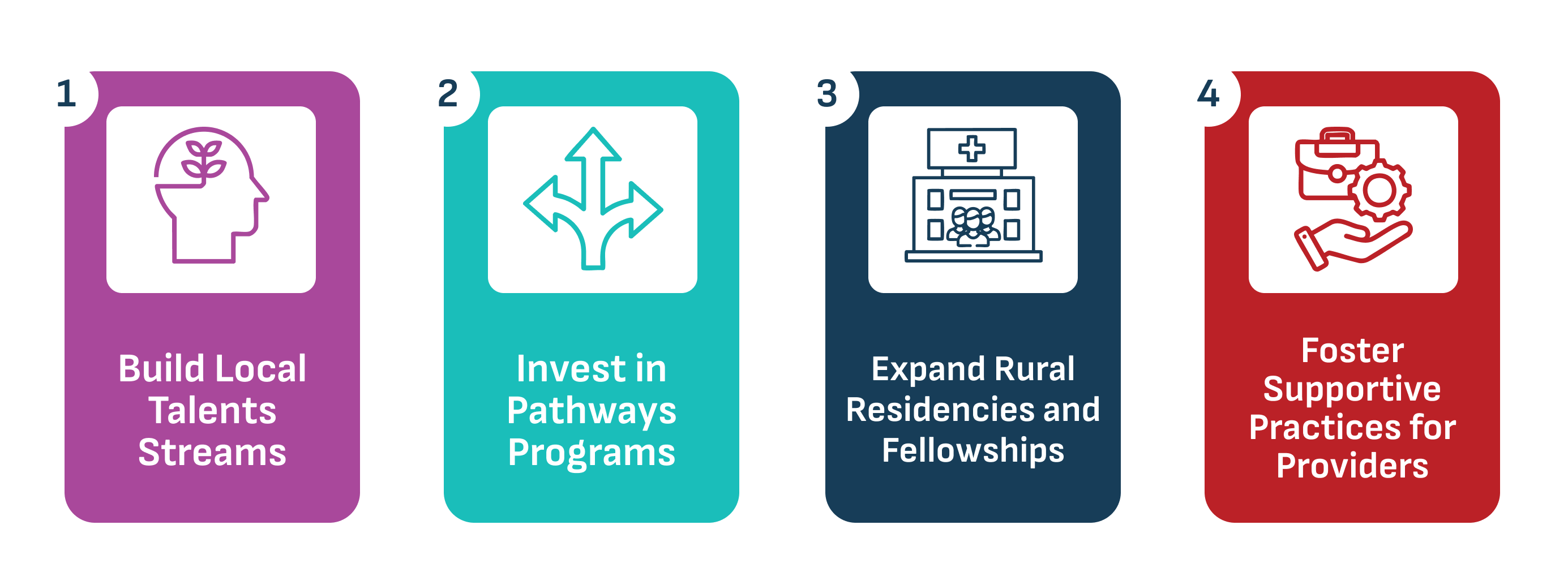
Below are effective, actionable approaches—grounded in Abt’s engagement findings and national evidence—that states and health centers can adopt and adapt.
Spotlight:
- An Indiana health center worked with community colleges on a “day in the life” program to introduce high school students to entry-level health care roles.
- An Alaska health center and their primary care association developed an apprenticeship program to train CHWs and MAs; many graduates now work at the center.
Spotlight:
- One health center boosted retention by funding staff training for career advancement with a minimal required work commitment. This included helping patient service representatives get an MA certification, MAs to become Licensed Practice Nurses (LPNs), and LPNs to become Registered Nurses.
- One behavioral health organization launched a Training-to-Practice Loan Support Program to provide partial loan repayment for clinical social workers while they are completing their supervised hours for licensure.
Spotlight:
- A health center in Michigan is working with medical schools to host third- and fourth-year rotations so students gain health center experience and view it as an option for their residency and career.
Spotlight:
- One health center found a team-based approach attracted new physicians who found an integrated, collaborative, and non-hierarchical approach more appealing than a more siloed environment.
How Abt Helps
Health centers work diligently to strengthen the health workforce, but they urgently need comprehensive, evidence-based solutions. Abt Global supports workforce development across the country by:
- Facilitating engagement, synthesizing insights, and translating them into workable implementation tools. We equip teams with practical templates, technical assistance, and policy options tailored to your context.
- Codesigning Grow-Your-Own toolkits, telehealth hub operating guides, and behavioral health integration checklists.
- Aligning workforce models, billing, and scope so teams can practice at the top of their license.
- Building apprenticeship programs, workforce resiliency strategies, and regional collaboratives that reduce individual burden and widen the pipeline.
Moving Forward
Building and sustaining a strong health workforce isn’t just about filling positions—it’s about creating pathways for growth, fostering collaboration, and investing in the future of rural health. The strategies outlined here demonstrate that innovation and partnership can turn workforce challenges into opportunities for resilience and impact.
Explore these approaches, share them with your teams, and reach out. Together, we can ensure that every community has access to the care it deserves.
Sources:
i. Commonwealth Fund. (2025, November 17). The state of rural primary care in the United States. https://www.commonwealthfund.org/publications/issue-briefs/2025/nov/state-rural-primary-care-united-states
ii. Rural Health Research Gateway. (2023, August). Rural Health Research RECAP: Rural Behavioral Health Workforce. https://www.ruralhealthresearch.org/assets/5373-24554/behavioral-health-workforce-recap.pdf
iii. HRSA Bureau of Health Workforce. (2024, November). State of the behavioral health workforce, 2024. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/state-of-the-behavioral-health-workforce-report-2024.pdf
iv. National Association of Community Health Centers. (2023, February). Closing the primary care gap: How community health centers can address the nation’s primary care crisis. https://www.nachc.org/wp-content/uploads/2023/06/Closing-the-Primary-Care-Gap_Full-Report_2023_digital-final.pdf
v. HRSA Data Warehouse. (2024). 2024 health center data. https://data.hrsa.gov/topics/healthcenters/uds/overview/national/table?tableName=Full&year=2024
vi. National Rural Health Association Policy Brief. (2025, March). Rural workforce recruitment and retention factors. https://www.ruralhealth.us/nationalruralhealth/media/documents/advocacy/nrha-policy-brief-workforce-retention-factors-final-3-7-25.pdf
vii. Patterson, D.G., Shipman, S. A., Pollack, S. W., Andrilla, C. H. A., Schmitz, D., Evans, D. V., Peterson, L. E., Longenecker, R. (2024). Growing a rural family physician workforce: The contributions of rural background and rural place of residency training. Health Services Research, 59(1), e14168. https://doi.org/10.1111/1475-6773.14168











